Background
While there is accumulating evidence that measurable residual disease (MRD) negative patients with intermediate risk AML may not benefit from allogeneic transplantation in 1 st complete remission (CR1-allo), many consider the presence of a FLT3 Internal Tandem Duplication (ITD) an indication for this procedure. However, the studies supporting this practice were mainly performed before the development of sensitive molecular MRD techniques (Schlenk NEJM 2008).The UK NCRI AML17 and AML19 trials studied, then incorporated, MRD by RT-qPCR into the management of patients with NPM1 mutated AML.
Methods
NCRI AML17 (April 2009 to December 2014) and AML19 (November 2015 to November 2020) were sequential prospective randomised trials for younger adults (18 - 60 years) with newly diagnosed AML. In AML17, decisions regarding CR1-allo were made using a validated risk score incorporating baseline factors and response to induction. In AML19, for patients with NPM1 mutated AML ( NPM1mut) the protocol recommended CR1-allo only in patients testing MRD positive in the peripheral blood (PB) post cycle 2 (PC2), regardless of other baseline risk factors such as FLT3 ITD, based on findings from AML17 (Ivey et al, NEJM 2016). Both trials were performed prior to the availability of midostaurin and FLT3 ITD MRD assays. Here we compare the outcomes of patients with NPM1mut in these trials and assess the benefit of CR1-allo according to FLT3 ITD and molecular MRD status. Time-to-event variables are analysed using the Kaplan-Meier method, and the impact of alloSCT assessed using time-dependent Cox regression and visualised with Simon-Makuch plots. Molecular relapses were included as relapse events, and alloSCT performed after molecular relapse was not considered as CR1.
Results
737 patients with NPM1mutAML who achieved CR/CRi and had a valid PC2 PB MRD result were included in the analysis. 60/348 (17%) patients from AML17 and 83/389 (21%) from AML19 tested PB PC2 MRD positive. Overall, CR1-allo was performed in 20% of patients in AML17 and 25% in AML19. Of the MRD positive patients CR1-allo was performed in 16/60 (27%) in AML17 compared to 50/83 (60%) in AML19 where these patients were recommended for transplant. CR1-allo was performed in 18% and 16% of MRD negative patients in AML17 and AML19 respectively.
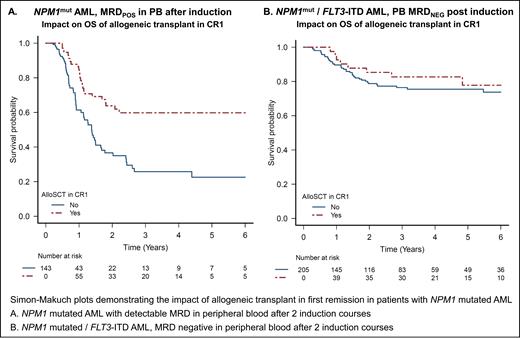
In AML17, as previously reported (Ivey et al, NEJM 2016), patients who were MRD+ had poor outcomes, with 3-year cumulative incidence of relapse (CIR) of 84% and overall survival (OS) of 25%. These outcomes were improved in AML19, with 3y CIR 50% and 3y OS 51%. Across both trials, CR1-allo was associated with a significant survival benefit in MRD+ patients (3y OS 61% vs 24%, HR 0.42, 95%CI 0.26-0.69, p<0.001, Figure A). Patients who were MRD negative had excellent outcomes in both trials (3y CIR 33% and 24% and 3y OS 75% and 83% for AML17 and AML19 respectively). AlloSCT in CR1 provided no survival advantage for MRD- patients (HR 0.83, 95%CI 0.51-1.34, p=0.4).
There were a total of 286 patients with NPM1mutFLT3 ITD mut AML with a PC2 PB MRD result across both trials. 81/286 (28%) were PB PC2 MRD+ of whom 32/81 (40%) received CR1-allo (28% in AML17 and 49% in AML19). Outcomes in these high-risk patients were improved in AML19, with 3y CIR 91% vs 68% and 3y OS 22% and 31% for AML17 and AML19 respectively. Those who received CR1-allo had improved outcomes (3y OS 45% vs 18%, HR 0.52, 95% CI 0.29-0.93, p=0.03) consistent with the overall MRD+ population.
In the 70% of NPM1mutFLT3 ITD mut AML patients who achieved PB PC2 MRD-, outcomes were encouraging in both AML17 (3y CIR 37%, 3y OS 75%) and AML19 (3y CIR 27%, 3y OS 80%). CR1-allo was performed in 20% (19% in AML17, 21% in AML19), with no survival benefit for transplant (HR 0.80, 95% CI 0.37-1.72, p=0.6, Figure B). There remained no benefit when restricted to those with high (>0.5) FLT3 ITD allelic ratio (HR 0.63, 95% CI 0.2 - 2.23, p = 0.50) and there was also no evidence of an interaction between allelic ratio and benefit from transplant for MRD negative patients (p=0.86).
Conclusion
Molecular MRD can be used to stratify decision making concerning post remission therapy in patients with NPM1mut AML. Patients who achieve MRD negativity in the peripheral blood by the end of course 2 are at low risk of relapse and we found no evidence of benefit from allogeneic transplant in CR1, including in the subset with FLT3 ITD. This finding contrasts with MRD+ patients where there was a significant survival benefit for CR1 transplant.
Disclosures
Freeman:JAZZ: Research Funding, Speakers Bureau; BMS: Research Funding; MPAACT: Membership on an entity's Board of Directors or advisory committees; NOVARTIS: Membership on an entity's Board of Directors or advisory committees, Speakers Bureau. Dillon:Astellas: Consultancy, Honoraria, Speakers Bureau; AvenCell: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees; Jazz: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding, Speakers Bureau; Novartis: Consultancy, Honoraria, Speakers Bureau; Pfizer: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding; Shattuck labs: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees; Amgen: Research Funding; Abbvie: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding, Speakers Bureau. Russell:Astellas: Honoraria; Servier: Honoraria; Jazz Pharma: Research Funding; Pfizer: Honoraria, Research Funding, Speakers Bureau.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal